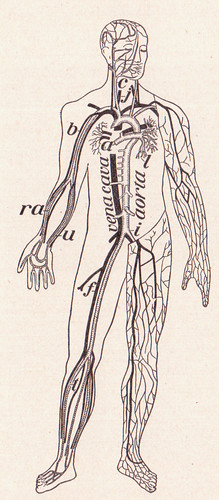
 We are without doubt one of the worlds most complicated machines. Our bodies are made up of trillions of cells, most of which contain a full copy of our own individual genome. Despite containing identical genetic information individual cells vary hugely in structure and function, for example, just think of the differences between skin and brain cells. This variation is achieved through the specialised way each cell reads it’s own copy of the genome, allowing cells to create only the components they require to function. One of the biggest challenges faced by biologists and medics today is bringing together our understanding of genes, gene processing, cellular and systems biology to gain a better understanding of how our bodies work, and what happens when things go wrong. Such research has lead us to appreciate just how individual we really are! It has highlighted how a combination of genes, environment and even our own compliment of bacteria can profoundly affect the way our cells function and ultimately our health. This ability to delve deeper into our inner workings has also spawned a new field of medicine known as personalised medicine.
We are without doubt one of the worlds most complicated machines. Our bodies are made up of trillions of cells, most of which contain a full copy of our own individual genome. Despite containing identical genetic information individual cells vary hugely in structure and function, for example, just think of the differences between skin and brain cells. This variation is achieved through the specialised way each cell reads it’s own copy of the genome, allowing cells to create only the components they require to function. One of the biggest challenges faced by biologists and medics today is bringing together our understanding of genes, gene processing, cellular and systems biology to gain a better understanding of how our bodies work, and what happens when things go wrong. Such research has lead us to appreciate just how individual we really are! It has highlighted how a combination of genes, environment and even our own compliment of bacteria can profoundly affect the way our cells function and ultimately our health. This ability to delve deeper into our inner workings has also spawned a new field of medicine known as personalised medicine.
Personalised medicine refers to the idea of tailoring treatment to an individual – the right drug or medical intervention for the right patient. In practice this doesn’t mean making a new se t of drugs for each individual, instead, it focuses on defining specific groups of people who are more or less likely to respond to treatment. Our current system relies on a ‘blanket’ method of treatment, i.e. everyone suffering from the same ailment will be treated with the same drugs/procedures. However, we now know that differences in genes and gene expression mean that individuals are unlikely to respond in the same way to medical treatments. This may go some way to explaining why between 30% and 70% of patients fail altogether to respond to drug treatment (1). It is ultimately hoped that a better understanding of how genes influence drug metabolism and function will improve both patient prognosis and reduce unnecessary spending on unsuccessful treatments. Indeed, progress is already being made towards a more personal approach to medicine:
t of drugs for each individual, instead, it focuses on defining specific groups of people who are more or less likely to respond to treatment. Our current system relies on a ‘blanket’ method of treatment, i.e. everyone suffering from the same ailment will be treated with the same drugs/procedures. However, we now know that differences in genes and gene expression mean that individuals are unlikely to respond in the same way to medical treatments. This may go some way to explaining why between 30% and 70% of patients fail altogether to respond to drug treatment (1). It is ultimately hoped that a better understanding of how genes influence drug metabolism and function will improve both patient prognosis and reduce unnecessary spending on unsuccessful treatments. Indeed, progress is already being made towards a more personal approach to medicine:
 One of the first major successes for personalised medicine came from the breast cancer drug Herceptin (Trastuzumab). In approximately 20% of invasive breast cancers a cell surface protein known as the HER is over produced causing cells to replicate uncontrollably. Screening tests have been produced to detect this defect and HER positive patients have been successfully treated with herceptin (an antibody which binds to the HER protein reducing cell replication). This breakthrough was soon followed by the discovery of a genetic abnormality, known as the Philadelphia translocation, associated with chronic myelogenous leukemia (CML). Since a high percentage of individuals with CML (~95%) also express this genetic abnormality, drugs targeted at blocking the protein produced by this abnormal gene were developed as a treatment. One of the most successful of these drugs (Gleevec) has now been FDA approved for the treatment of ten different cancers. These findings show how patient-specific genetic information can lead to improved health outcomes and novel therapeutics.
One of the first major successes for personalised medicine came from the breast cancer drug Herceptin (Trastuzumab). In approximately 20% of invasive breast cancers a cell surface protein known as the HER is over produced causing cells to replicate uncontrollably. Screening tests have been produced to detect this defect and HER positive patients have been successfully treated with herceptin (an antibody which binds to the HER protein reducing cell replication). This breakthrough was soon followed by the discovery of a genetic abnormality, known as the Philadelphia translocation, associated with chronic myelogenous leukemia (CML). Since a high percentage of individuals with CML (~95%) also express this genetic abnormality, drugs targeted at blocking the protein produced by this abnormal gene were developed as a treatment. One of the most successful of these drugs (Gleevec) has now been FDA approved for the treatment of ten different cancers. These findings show how patient-specific genetic information can lead to improved health outcomes and novel therapeutics.
 The scope of personalised medicine is not limited to drug development, it is also being used to assess the long term prognosis and treatment requirements of some cancer patients. A number of genetic screens have been developed to assess the likelihood of tumour recurrence following initial treatment in certain types of breast cancer. One of the more widely used tests, Oncotype DX, assesses 21 different genes found in tumour cells and, from these, predicts the likelihood of regrowth. This means that patients with low recurrence scores, therefore good prognosis, can be saved the stress of further unnecessary therapy and the healthcare system saves on the cost of providing unnecessary treatment. The success of this predictive screen has lead to further research into similar screening for other types of cancer and it is hoped that these tests will soon be widely available as predictive tools.
The scope of personalised medicine is not limited to drug development, it is also being used to assess the long term prognosis and treatment requirements of some cancer patients. A number of genetic screens have been developed to assess the likelihood of tumour recurrence following initial treatment in certain types of breast cancer. One of the more widely used tests, Oncotype DX, assesses 21 different genes found in tumour cells and, from these, predicts the likelihood of regrowth. This means that patients with low recurrence scores, therefore good prognosis, can be saved the stress of further unnecessary therapy and the healthcare system saves on the cost of providing unnecessary treatment. The success of this predictive screen has lead to further research into similar screening for other types of cancer and it is hoped that these tests will soon be widely available as predictive tools.
Beyond cancer, personalised medicine is also being investigated as a way of understanding the adverse side effects linked with certain drug treatments. Current research has highlighted a number of genes associated with drug hypersensitivity and variations in metabolism. It is hoped that this knowledge will, in the future, allow doctors to predict which individuals are more likely to experience adverse side effects to during treatment and tailor their prescriptions and doses accordingly.
However, despite these successes, personalised medicine still has a long way to go before its full potential can be realised. One of the first and arguably most important challenges facing this field will be defining which genetic and cellular abnormalities lead to disease. In a small number of cases this has already been achieved, for example we know exactly what gene leads to to cystic fibrosis. However most disorders are more complex, stemming from abnormalities an any of a number of different genes. Therefore uncovering the precise risk factors for these disorders will require a staggering amount of data from a huge number of individuals. Also, just to make things a bit more complicated, the emerging field of ‘epigenetics’ is now challenging the belief that we are simply the sum of our genes.
[youtube http://www.youtube.com/watch?v=kp1bZEUgqVI]
Epigenetics is revealing how interactions with the environment can change the way our cells read our genetic code. This means that two people with identical genes could still suffer from very different ailments depending on what environmental factors they are exposed to. Finally it is important to consider the ethical implications of these procedures, i.e. data protection, patient confidentiality and access to (perhaps costly) personalised treatments (this is discussed in more depth here).
Although certainly challenging, I don’t think these problems are insurmountable and the gains of personalised treatments will certainly be worth the scientific investment. Therefore, with continued funding and research effort I hope it is only a matter of time before we see more personalised diagnosis and treatment available to the wider public.
Post by: Sarah Fox
(1): Progress towards personalized medicine, Stewart Bates, Drug Discovery Today 2010. Subscription required for full access.