 Ketamine is probably best known as a recreational drug and horse tranquilliser. However, it also has a number of beneficial medical uses. It is routinely used as an anaesthetic, it is used in medical research to replicate symptoms of schizophrenia and current work suggests it may also be an effective treatment for depression. So what do we know about ketamine and how could a popular psychedelic drug be used to treat a psychiatric disease?
Ketamine is probably best known as a recreational drug and horse tranquilliser. However, it also has a number of beneficial medical uses. It is routinely used as an anaesthetic, it is used in medical research to replicate symptoms of schizophrenia and current work suggests it may also be an effective treatment for depression. So what do we know about ketamine and how could a popular psychedelic drug be used to treat a psychiatric disease?
Why take ketamine?
Ketamine is classed as a psychotomimetic: this means it can induce hallucinations , delusions and feelings of dissociation from the world around you (other examples of psychomimetics include LSD and cannabis). These effects make ketamine a desirable recreational drug, but they are not the drug’s only action. It can also cause people to appear unresponsive or apathetic, severely disrupt memory and concentration and, at high doses, even lead to temporary paralysis or coma. Because these effects are similar to the symptoms of schizophrenia, it is commonly administered to rats (and healthy human volunteers) to study schizophrenia and test potential new drugs.
, delusions and feelings of dissociation from the world around you (other examples of psychomimetics include LSD and cannabis). These effects make ketamine a desirable recreational drug, but they are not the drug’s only action. It can also cause people to appear unresponsive or apathetic, severely disrupt memory and concentration and, at high doses, even lead to temporary paralysis or coma. Because these effects are similar to the symptoms of schizophrenia, it is commonly administered to rats (and healthy human volunteers) to study schizophrenia and test potential new drugs.
Ketamine produces its psychotic effects by disrupting the way the brain perceives the world and how it processes information. Specifically, it blocks the transmission of signals between a group of neurons which use the neurotransmitter glutamate (a chemical signal that neurones use to communicate). It does this by selectively interfering with the regions of the cell which detect glutamate; acting preferentially in certain parts of the brain, such as the prefrontal cortex.
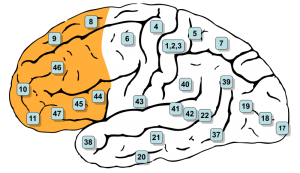
The prefrontal cortex, at the front of the brain, is responsible for higher functions; such as problem-solving, reasoning, understanding social interactions and control of behaviour. This region is important for enabling us to understand the world around us and make decisions about how to interact with it. Activity in the prefrontal cortex is managed by ‘inhibitory’ neurons (cells that prevent other neurones becoming too excited). These cells control what signals the prefrontal cortex sends to other brain regions. Ketamine selectively targets these inhibitory neurons, making them less active. This allows activity in the prefrontal cortex to continue unchecked, leading to disorganised communication and a disruption of its communication with other brain regions. The signals coming out of the prefrontal cortex make less sense and more irrelevant information is transmitted.
This extra transmission of irrelevant information may be crucial to understanding the basis of delusional thinking. If normally uninteresting stimuli are flagged up by the brain as important, this could prevent the brain from making sense of the world in a normal way, leading to bizarre or irrational beliefs and disorganised thoughts.
The effects of ketamine are fairly short-lasting: in clinical studies effects usually wear off within a few hours. Regular use may, however, have longer-lasting effects on the brain and reports of users developing psychological dependence have increased in recent years.
Ketamine for depression
 Recently a number of clinical trials have found that a single low dose of ketamine can improve the symptoms of depression in a matter of hours. These trials used volunteers suffering from severe depression that had previously shown no improvement with traditional anti-depressants. Within 24 hours of a single dose, the percentage of patients showing a considerable improvement in mood varied across trials from 25% to an impressive 85%. Some patients showed improvements that lasted for weeks, however the majority of patients showed improvement lasting only a few days. Compared with the usually prescribed anti-depressants, this is an incredibly fast response; most take weeks to act, and can actually worsen symptoms before they show beneficial effects. This is an exciting development, especially for the treatment of suicidal patients, where rapid treatment is essential. Importantly, side-effects are generally mild, because the dose is far lower than a typical recreational dose.
Recently a number of clinical trials have found that a single low dose of ketamine can improve the symptoms of depression in a matter of hours. These trials used volunteers suffering from severe depression that had previously shown no improvement with traditional anti-depressants. Within 24 hours of a single dose, the percentage of patients showing a considerable improvement in mood varied across trials from 25% to an impressive 85%. Some patients showed improvements that lasted for weeks, however the majority of patients showed improvement lasting only a few days. Compared with the usually prescribed anti-depressants, this is an incredibly fast response; most take weeks to act, and can actually worsen symptoms before they show beneficial effects. This is an exciting development, especially for the treatment of suicidal patients, where rapid treatment is essential. Importantly, side-effects are generally mild, because the dose is far lower than a typical recreational dose.
It isn’t clear what causes ketamine’s anti-depressant effects but it isn’t thought to be a direct result of alteration in neuronal communication. In healthy subjects, small amounts of ketamine doesn’t influence mood, indicating that it may act to correct some problems found specifically in depressed patients. One possibility is that it encourages new connections to be created between neurons. This may be beneficial since research has found reduced numbers of connections in the brains of depressed patients.
However, this research is still in the early stages. The next big challenge is to determine a schedule of treatment to maintain the short-term improvements seen after one dose. This may involve combining ketamine with other anti-depressants, or repeating the dose. Although further research is still needed to assess the long-term effects of ketamine as an anti-depressant.
These exciting results suggest that in the future, ketamine may be famous not as a club-drug or horse-tranquilliser, but as a life-changing treatment for a devastating mental condition.
Post by: Claire Scofield
Interesting read… seems like people are self medicating with these drugs of ‘abuse’ for a reason; Prof. Nutt recently posited that psilocybin is also of potential benefit for depression and of course the proven benefits of MDMA for PTSD.
Ketamine has saved my life if I hadn’t found it as a treatment option at a low dose, I would’ve been dead already
There is a community of RSD/CRPS sufferers that are using, interested in the treatments of ketamine. These are the worst cases & the side effects seem to outweigh the positive effects. Is this something you would want your child to experience? I don’t know. Very interesting even if I was a horse!
F*ckin’ remarkable things here. I am very happy to peer your article.
Thanks a lot and i am taking a look forward to touch you.
Will you please drop me a mail?