How does an infection affect the progression of Alzheimer’s disease?

Alzheimer’s disease (AD) is the most common form of dementia. It’s a neurodegenerative condition characterized by ongoing cognitive decline, loss of functions such as memory, and behavioural abnormalities. AD usually occurs amongst the elderly, and its prevalence is now so high, that its estimated overall cost to society is 5 times that of cancer, heart disease and stroke. While AD was first identified over a century ago, research into its causes has only really begun to gather momentum over the past 30 years. Some think that damage may stem from the formation of toxic ‘plaques’ and ‘tangles’ that appear to be associated with brain cell death. Unfortunately, understanding the triggers of neurodegeneration has become a much more troublesome challenge.
Some teams have begun to look at the contribution of inflammation to the development of brain atrophy (shrinkage). Inflammation is the first response of the immune system to infection/injury. You can recognise inflammation when you graze your skin or sprain an ankle: as well as pain, there may be redness, swelling and the area may feel hot to the touch. This is thanks to the extra blood carrying immune cells to the site of injury to prevent infection and aid repair. The inflammatory response is an innate and usually protective reaction to injury or infection and requires the co-operation between local, ‘resident’ immune cells at the site of injury and circulating immune cells in the bloodstream.
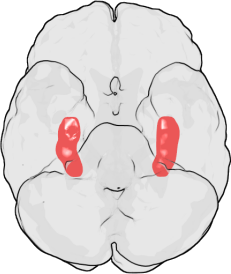
The main resident immune cells of the brain are called microglia; they respond to infection and injury to trigger an inflammatory response. Microglia are hyper-sensitive to changes in their local environment. When the brain is injured, they become ‘activated’. They change shape and behave differently, releasing different chemicals which can be toxic to brain cells. Some research has suggested that it’s possible that activated microglia break down the connections between cells in the memory centre of the brain, the hippocampus. Intriguingly, hippocampal damage and memory loss are the primary symptoms of AD.
Several lines of evidence have implicated microglial inflammation in AD, including the observation of activated microglia in the brains with Alzheimer’s, and the possibility that anti-inflammatory drugs may be neuroprotective. However, clinical trials have failed to show any efficacy yet.
Professor Hugh Perry and his research group at the University of Southampton investigate how inflammation contributes to outcome of brain diseases. About ten years ago Perry and his team developed an animal model (the prion mouse) to better understand the complex role of inflammation in AD. A chemical that causes neurodegeneration was injected into the mouse hippocampus (the memory centre of the brain), and the researchers studied the evolution of the resulting prion disease, which bears some similarities to AD. Thirteen weeks after the injection, although the mice appeared normal, there were more activated microglia found in the hippocampus, even compared to surrounding areas of the brain. The researchers then claimed that this microglial activation was pathological, since the mice showed some behavioural disturbances and deficits in learning tasks.
Perry and his team suggested that systemic infections in patients with AD could worsen cell death in the brain, speeding up neuron deterioration and memory loss. (‘Systemic’ infections are so-named because they infect a number of organs and tissues or affect the body ‘system’ as a whole, instead of being localized in one area.)
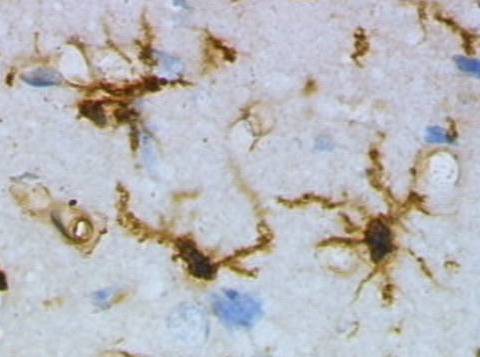
 Resting (top) and activated (bottom) rat microglia after a brain injury. Images by Grzegorz Wicher (Wikicommons).
Resting (top) and activated (bottom) rat microglia after a brain injury. Images by Grzegorz Wicher (Wikicommons).To look into this idea, researchers looked at differences between the prion mouse with an ‘infection’ (or rather, an injection of a toxin released by bacteria to mimic an infection) or without infection. The prion mouse given a fake infection had twice as many dead brain cells as the uninfected prion mouse. Researchers concluded that the microglia are primed by the ongoing prion disease and so, when the infection is added, they overreact. They then drive the production of a number of inflammatory chemicals, which triggers a whole host of damaging effects on brain cells.
Perry and his team collaborated with other research groups to identify whether the evidence they had gathered would be relevant to AD patients. In a small pilot study of 85 AD patients with moderate cognitive impairment scores over 2 months, they found that those who had infections showed a more cognitive decline than the other patients in the study. This was the first evidence in a clinical setting that systemic infection may affect neurological disease progression. The next study involved 300 AD patients, 50% of whom had a systemic infection within the recorded 6 months. The researchers saw that patients that got an infection within the 6 months suffered three times the rate of cognitive decline, compared to a small cognitive decline in those who had not had an infection.
These fascinating studies have provided the first clinical evidence that as well as inflammation in the brain driving damage, infection and inflammation in the body can also worsen and speed up neurodegeneration. It appears that brain-resident microglia become primed for activation, so that when patients suffer from a bodily infection, their brain cells become more vulnerable to the damaging effects of an inflammatory response.
Not only did this research provide ideas to potentially help AD patients today, but it also formed the basis for an important direction for current disease research. The evidence on the highly complex interplay between the diseased brain and systemic inflammation can be applied, not just to AD, but as a generic concept to many nervous system diseases.
Post by Isabelle Abbey-Vital
To whom it may concern:
I would like to share with you an article, if you have not seen it yet, which may reinforce the work that you have done. I became aware of it because I am being treated for Lyme disease. I reside in Chicago, Illinois, USA. The article is by the neurologist J. Miklossy, and is based on a meta-analysis of research papers. She finds that 90% of autopsied Alzheimer brains are infected with pathogenic spirochetal bacteria (syphilis also is caused by a spirochetal bacterium, and is known to cause dementia in its final stage). Of this 90%, the Lyme spirochete accounted for 25%, and the remaining 65% consisted of pathogenic oral spirochetes which originated in the mouth and made their way to the brain either through the blood stream or by way of nerve pathways between the mouth and brain. Other findings of the paper are that the bacterial infection is colocated with the A-Beta plaques, and that A-Beta itself is an anti-microbial protein, thus suggesting that it may be a physiological response to infection. Additionally, mammalian neural cells were cultured with the Lyme spirochetal bacteria, and the characteristic pathological features of Alzheimers were seen to result.
The full article can be found at:
http://www.ncbi.nlm.nih.gov/pubmed/21816039
Thank you and best wishes for continued progress in the fight against AD.
Sincerely,
Peter Kraus
Some genuinely interesting information, well written and
loosely user pleasant.
detiksport Informasi Berita Seputar Dunia Olahraga Terupdate •
Informasi Berita Olahraga Terbaru, Hasil Pertandingan, Klasemen, Jadwal Pertandingan,
Gosip Lapangan Detik Sport
Thanks so much for giving everyone remarkably memorable
chance to read articles and blog posts from this website.
It is often so brilliant and as well , packed with
fun for me and my office peers to visit your website at
the least three times in a week to read the new
guides you have got. Of course, I am also at all times
satisfied with all the unbelievable hints you give.
Certain 2 areas in this article are unequivocally the most
beneficial we have all had.