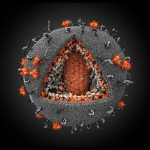
 With over 30 million sufferers worldwide, HIV remains the world’s leading infectious killer. The human immunodeficiency virus attacks the immune system, leaving it unable to fight infections, resulting in AIDS. Improving HIV care is one of the top 10 global health priorities. Therefore, when research published last year suggested a baby had been “cured” of HIV; tabloids quickly began to speculate, with some implying the elusive cure may be closer than we imagined. One year on, with similar cases set to be presented at AIDS 2014, the leading international conference on AIDS, what is the significance of this major breakthrough in terms of tackling the large-scale HIV pandemic?
With over 30 million sufferers worldwide, HIV remains the world’s leading infectious killer. The human immunodeficiency virus attacks the immune system, leaving it unable to fight infections, resulting in AIDS. Improving HIV care is one of the top 10 global health priorities. Therefore, when research published last year suggested a baby had been “cured” of HIV; tabloids quickly began to speculate, with some implying the elusive cure may be closer than we imagined. One year on, with similar cases set to be presented at AIDS 2014, the leading international conference on AIDS, what is the significance of this major breakthrough in terms of tackling the large-scale HIV pandemic?
“Absence of Detectable HIV-1 Viremia after Treatment Cessation in an Infant”
 In 2010, a baby was born prematurely to a mother whose HIV was only discovered during delivery. With no prenatal care, and therefore a high risk of exposure to the virus, the gutsy call was made to begin aggressive treatment with a combination of three antiretroviral drugs at just 30 hours old. Infection was confirmed soon after and the child remained receiving therapy.
In 2010, a baby was born prematurely to a mother whose HIV was only discovered during delivery. With no prenatal care, and therefore a high risk of exposure to the virus, the gutsy call was made to begin aggressive treatment with a combination of three antiretroviral drugs at just 30 hours old. Infection was confirmed soon after and the child remained receiving therapy.
Surprisingly, within days the level of HIV had rapidly diminished and within a month was non-detectable. However, the successful therapy was unexpectedly ceased after 18 months as the mother stopped taking the child to scheduled appointments. When the child was finally examined again, at 23 months, she remained free from infection despite not being on HIV medication. At the time of the paper the child continued to be in remission, gaining the title “the baby cured of HIV”.
Impact on cases involving babies born with HIV
 The doctors quickly emphasised the therapy proposed was a “functional cure”. With the child recently beginning to shown early signs of infection, it appears the treatment silenced the virus for a substantial period of time rather than eliminating it. In reality, cases involving mother-to-baby transmission are rare. Standard HIV pre-natal treatment can lower the risk to 2%. Therefore in areas where there are a significantly higher number of cases, such as Sub-Saharan Africa, the main factor is the sub-standard levels of health care rather than the need for new treatment.
The doctors quickly emphasised the therapy proposed was a “functional cure”. With the child recently beginning to shown early signs of infection, it appears the treatment silenced the virus for a substantial period of time rather than eliminating it. In reality, cases involving mother-to-baby transmission are rare. Standard HIV pre-natal treatment can lower the risk to 2%. Therefore in areas where there are a significantly higher number of cases, such as Sub-Saharan Africa, the main factor is the sub-standard levels of health care rather than the need for new treatment.
Is a new, miraculous treatment now available?
 The therapy itself wasn’t novel as it used readily available antiretroviral drugs; the “novel” aspect of the therapy was the early approach. This is already known to be advantageous as early aggressive treatment is thought to prevent viral reservoirs forming. HIV reservoirs are what hide the virus, making it resistant to the both the immune system and medication, and form within hours of infection.
The therapy itself wasn’t novel as it used readily available antiretroviral drugs; the “novel” aspect of the therapy was the early approach. This is already known to be advantageous as early aggressive treatment is thought to prevent viral reservoirs forming. HIV reservoirs are what hide the virus, making it resistant to the both the immune system and medication, and form within hours of infection.
Can adults now be cured of HIV?
There has been speculation that the immune response of a newborn is more suited to cope with HIV than an adults. Not only are babies immune systems immature, resulting in a milder reaction to the virus, but they lack the memory “defender” cells that are the target of the dangerous viral reservoirs. However, last year several adults were reported to have undergone a similar “functional cure”. Having undergone early antiretroviral treatment, 14 out of 70 patients remained virus free for at least 3 years, following cessation of therapy. This suggests that 5%-15% of HIV patients could eradicate the virus through early treatment.
Early treatment plans would not benefit current sufferers but could help tackle new cases. While treating the virus as soon as possible seems like an obvious idea, it appears it would be difficult to implement. Not only do 1 in 5 sufferers remain unaware they are infected, but the stigma associated with HIV means many people are reluctant to get tested. Therefore, before getting excited over the potential of early treatment regimes, the bigger challenge of identifying the infection promptly needs to be addressed.
The “functional cure” has provided hope and opened new areas for scientists to explore. Importantly, it strengthened the idea that early treatment is vital. However bigger social and development issues, involving improving health care in poorer societies and ensuring early identification, need to be addressed before the findings can be translated into the “HIV cure” that has been widely speculated.
Post by: Claire Wilson
References
Persaud, D., et al., Absence of Detectable HIV-1 Viremia after Treatment Cessation in an Infant. New England Journal of Medicine, 2013. 369(19): p. 1828-1835.
Saez-Cirion, A., et al., Post-Treatment HIV-1 Controllers with a Long-Term Virological Remission after the Interruption of Early Initiated Antiretroviral Therapy ANRS VISCONTI Study. Plos Pathogens, 2013. 9(3).